Pain is not just a sensation,
it’s a complex experience influenced by multiple brain regions. Traditional pain assessment methods rely on subjective descriptions, making diagnosis and treatment inconsistent.
At PainSense, we are revolutionizing pain assessment by leveraging objective data and scientific advancements. Understanding how pain is processed in the brain helps us develop better solutions for both patients and healthcare providers.
This article explores how supraspinal regions play a role in pain processing and how PainSense’s technology is shaping the future of pain management.

What Are Supraspinal Regions in Pain Processing?
Supraspinal regions refer to key brain structures that contribute to pain perception, modulation, and response. These regions work together to interpret pain signals, regulate emotional responses, and influence treatment effectiveness.
Pain is not just a physical reaction—it is shaped by emotions, cognition, and past experiences. This explains why two people with the same injury can experience pain differently.

Key Supraspinal Regions in Pain Perception
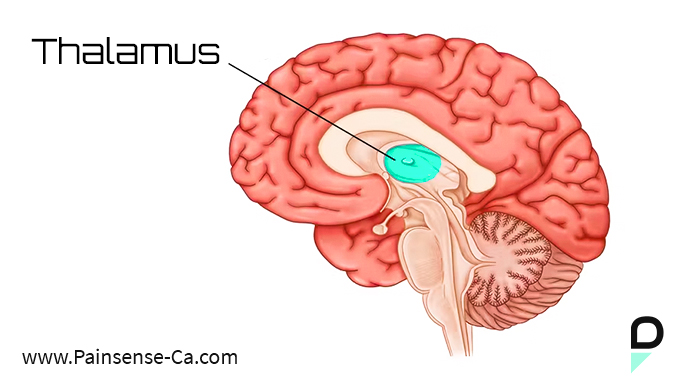
1. Thalamus
The Pain Relay Center
The thalamus acts as the brain’s sensory hub, receiving pain signals from the spinal cord and directing them to higher brain regions.
- Determines pain intensity and location.
- Filters pain signals, deciding which sensations need attention.
How PainSense Helps: By integrating objective pain data, PainSense ensures that pain reporting is accurate and measurable, eliminating the limitations of subjective pain scales.
2. Somatosensory Cortex
Mapping Pain Sensations
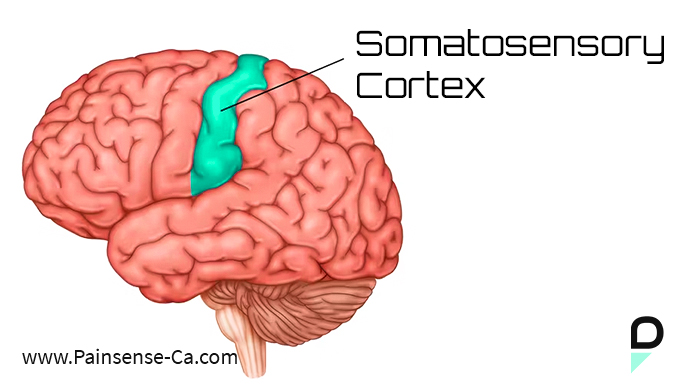
The somatosensory cortex helps the brain interpret pain in a detailed and localized way.
- Identifies where pain is felt and its type (sharp, dull, burning).
- Works with the thalamus to pinpoint pain sources.
PainSense’s Impact: Our technology provides healthcare professionals with clear, data-driven insights into a patient’s pain levels, allowing for more precise and targeted treatments.
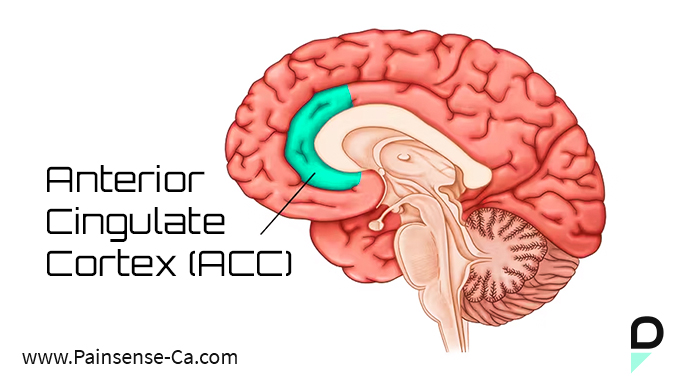
3. Anterior Cingulate Cortex (ACC)
Emotional Connection to Pain
The ACC is responsible for the emotional distress associated with pain. This explains why pain often triggers feelings of frustration, anxiety, or fear.
- Regulates emotional responses to pain.
- Overactivity in the ACC is linked to chronic pain conditions.
PainSense’s Approach: By offering objective pain assessment, PainSense helps reduce uncertainty in treatment plans, which can lower anxiety levels for patients experiencing chronic pain.
4. Insular Cortex
The Pain Awareness Center
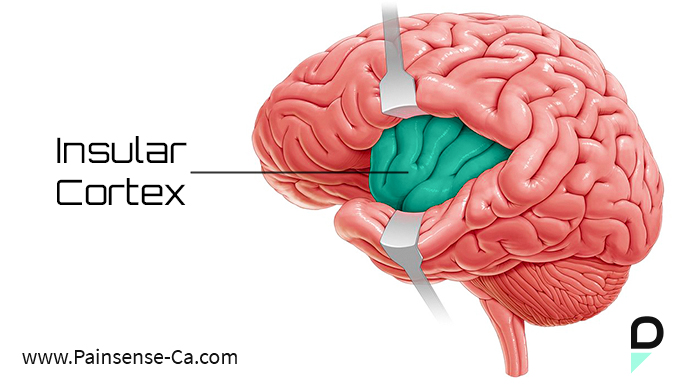
The insula integrates sensory, emotional, and autonomic responses to pain.
- Helps perceive pain intensity.
Connects pain with heart rate, blood pressure, and stress responses.
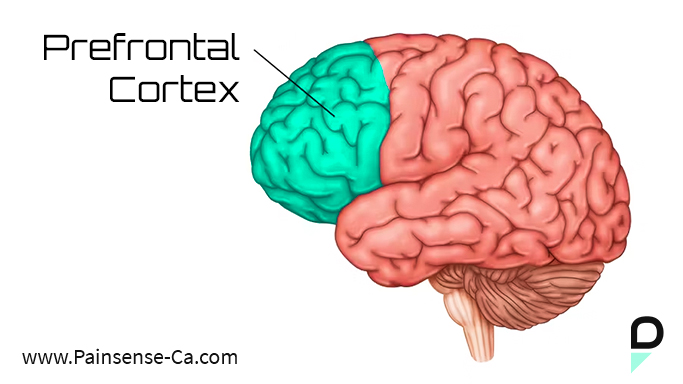
5. Prefrontal Cortex (PFC)
Regulating Pain Perception
The prefrontal cortex helps interpret and cope with pain.
- Modifies pain perception based on past experiences.
- Plays a role in distraction and pain tolerance.
By providing data-backed insights, our technology helps clinicians tailor treatments based on objective pain trends rather than subjective reports.
6. Periaqueductal Gray (PAG)
The Brain’s Painkiller System
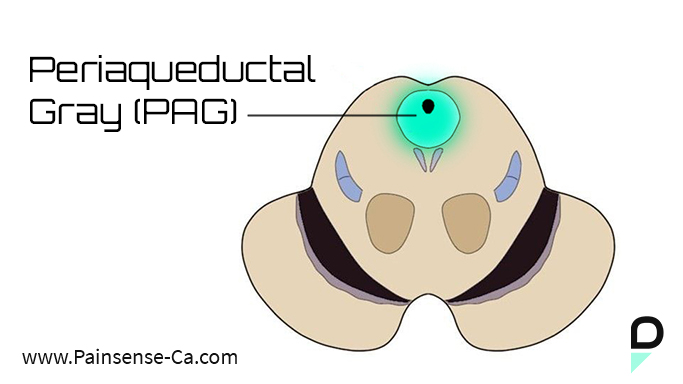
The prefrontal cortex helps interpret and cope with pain.
- Modifies pain perception based on past experiences.
- Plays a role in distraction and pain tolerance.
PainSense’s Role: By providing data-backed insights, our technology helps clinicians tailor treatments based on objective pain trends rather than subjective reports.
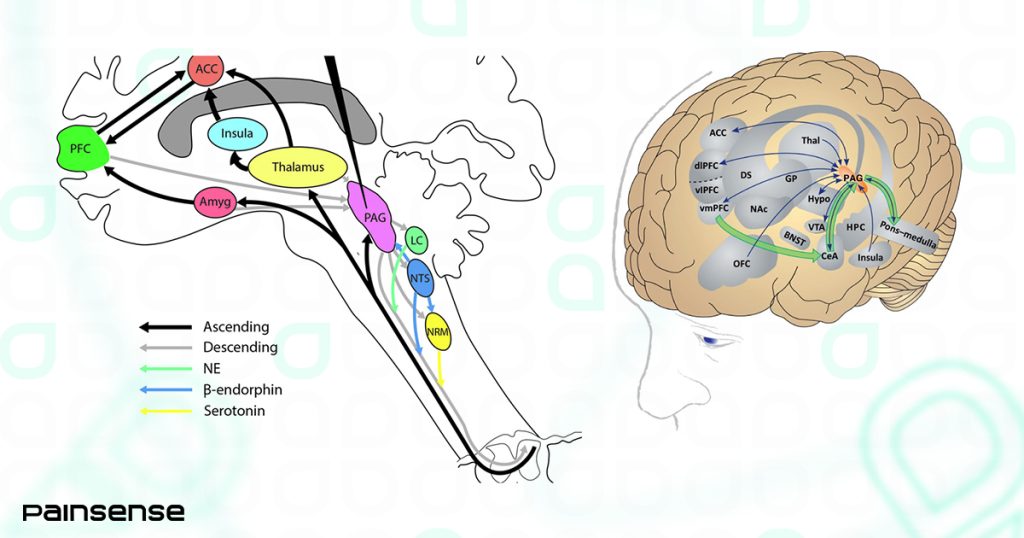
How These Regions Work Together
Pain perception is not a linear process…,
it’s a complex network of interactions between sensory, emotional, and cognitive pathways.
- The thalamus relays pain signals to the somatosensory cortex for processing.
- The ACC and amygdala attach emotional significance to pain.
- The insula helps interpret pain intensity and awareness.
- The PFC and PAG regulate pain, increasing or decreasing perception based on context.
This pain matrix highlights why a one-size-fits-all pain treatment doesn’t work, individuals process pain differently based on their brain’s activity.
Chronic Pain and Brain Plasticity
Chronic pain can rewire the brain, leading to long-term changes in supraspinal regions.
- Overactivity in the amygdala can lead to increased pain sensitivity.
- Reduced function in the PFC and PAG can limit natural pain suppression.
- Increased ACC and insular cortex activity can heighten pain perception.
PainSense helps combat this challenge by providing consistent, measurable pain data, enabling clinicians to track pain patterns over time.
PainSense: The Future of Pain Assessment
Advancements in neuroscience are reshaping how we approach pain management. PainSense is leading this movement by offering:
- Objective pain measurement through cutting-edge technology.
- Data-driven insights that enhance treatment plans.
- A patient-centered approach to improve healthcare outcomes.
By understanding how pain is processed in the brain, PainSense empowers both patients and healthcare professionals to make informed, effective decisions.
Pain is not just a sensation, it is a complex experience shaped by multiple brain regions. From sensory processing in the thalamus to emotional regulation in the ACC, pain perception is unique to every individual.
At PainSense, we are dedicated to bridging the gap between neuroscience and pain management by providing objective, accurate, and innovative solutions for assessing pain.
Want to learn more about how PainSense is transforming pain assessment? Visit us at Painsense-ca.com