The Foundation of Effective Care: Why Pain Assessment Matters
Pain is one of the most common reasons patients seek medical care — yet paradoxically, it remains one of the hardest experiences to measure accurately. Every day, clinicians in oral and maxillofacial surgery, emergency medicine, dentistry, oncology, and rehabilitation face the same question: how can we quantify something so deeply subjective?
Traditional tools like the Visual Analogue Scale (VAS) and Numeric Rating Scale (NRS) have been the backbone of clinical pain assessment for decades. They’re quick, simple, and standardized, but they also rely entirely on patient self-reporting. These scales assume that every patient can articulate their pain in numbers or words, which is rarely the case in real-world healthcare settings.
A patient’s mood, anxiety level, cultural background, and even momentary stress can influence their self-assessed pain score.
Research has shown that these factors can lead to wide discrepancies: two patients experiencing similar physiological pain may report very different numbers on the same scale. This makes clinical interpretation difficult, especially for post-operative monitoring or chronic pain management.
For clinicians, that uncertainty can have serious consequences.
Underestimating pain can delay recovery and reduce trust between patient and provider.
Overestimating pain can lead to unnecessary medication, prolonged opioid use, or additional procedures.
In both cases, the lack of precision in pain measurement directly impacts the quality of care. As a result, pain management often depends on experience and intuition rather than consistent, objective data — a reality that leaves significant room for improvement.
This is where objective, data-driven pain assessment becomes essential. By using quantifiable physiological or behavioral indicators, clinicians can make informed decisions that reduce guesswork and bias. In recent years, advances in medical technology, AI, and biosensor research have made it possible to move beyond subjective scales and toward more standardized, reproducible pain data. These developments are already transforming how we think about pain, particularly in post-surgical care and rehabilitation settings.
At PainSense, we are tackling this challenge head-on. Our mission is simple yet transformative: to make pain measurable in real, quantifiable terms. A shift from subjective perception to objective insight. We believe that when clinicians can measure pain with precision, they can treat it more effectively, improve patient comfort, and optimize care outcomes across every specialty.
This philosophy guides every aspect of our work, from the development of our MVP device to our ongoing research collaborations in Canada. It also underpins our broader mission to enhance the tools available to physicians, surgeons, and researchers around the world.
You can read more about our approach and how we’re advancing this field in our previous article, Latest Advancements of Pain Assessment Tech.
Together, these innovations mark the beginning of a new era in healthcare, one where pain is no longer just felt or described, but measured, understood, and managed with the accuracy it deserves.

How PainSense Is Changing the Landscape of Pain Assessment
Our solution is built on a simple yet powerful concept:
Pain is not just a feeling;
It’s a physiological and behavioral response that can be measured and analyzed. PainSense’s device allows patients to communicate their pain through a physical action, such as applying pressure to a calibrated sensor. The device then converts that input into a reliable pain intensity score, creating an objective data point clinicians can use alongside traditional methods.
Unlike the subjective nature of conventional scales, our system translates pain into a consistent numerical value, independent of linguistic or emotional bias. This means healthcare providers can:
Quantify pain objectively rather than relying solely on verbal reports.
Track changes in real time, observing whether interventions truly reduce pain.
Enhance communication between patients and providers, especially in pediatric, geriatric, or non-verbal populations.
Standardize documentation of pain in electronic health records for research and outcome evaluation.
For oral and maxillofacial surgeons, anesthesiologists, and post-operative care specialists, PainSense represents a step toward the next generation of patient monitoring, where subjective interpretation gives way to clinical precision.

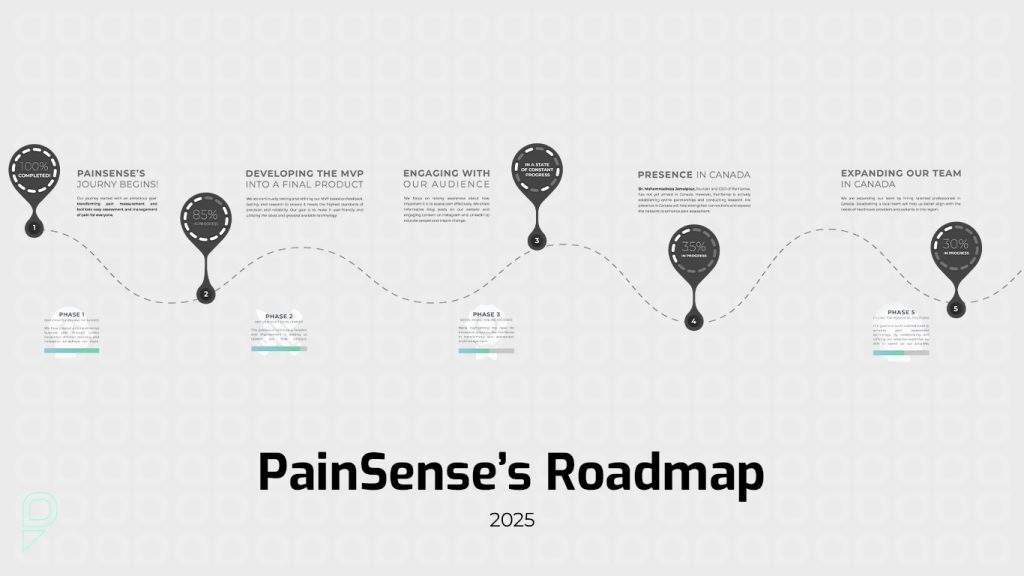
Our Roadmap: From Prototype to Real-World Impact
Finalizing Our MVP
We are in the final stages of completing our Minimum Viable Product (MVP), the first fully functional version of the PainSense device. Our engineering and research teams have refined the prototype into a compact, ergonomic tool designed for clinical reliability and patient comfort. The MVP will form the backbone of our early pilot studies and collaborations with healthcare institutions.
Expanding Our Research in Canada
A major milestone in our journey is the approval of Dr. Mohammad Reza Jamalpour’s Canadian work permit. This will allow him to continue his research directly within the Canadian healthcare ecosystem, collaborating with local hospitals, universities, and clinicians. His on-site presence will be instrumental in validating the device under real-world clinical conditions.
Dr. Jamalpour brings over 20 years of experience as an oral and maxillofacial surgeon and university professor. His deep understanding of pain dynamics — particularly in surgical and post-operative contexts — has shaped the vision behind PainSense. With his relocation to Canada, we are entering a new phase of scientific and professional growth.
Growing Our Community and Team
We’ve built an active presence on social media [Instagram and LinkedIn] where we share research insights, MVP updates, and behind-the-scenes moments from our innovation journey.
As our work accelerates, we will soon be hiring locally in Canada. PainSense aims to collaborate with talented Canadian professionals, from biomedical engineers and product designers to marketing and clinical support specialists, who share our passion for healthcare innovation.

Why We Chose Canada
When deciding where to grow PainSense globally, Canada stood out for several reasons.
1. A Thriving MedTech Ecosystem
Canada’s healthcare innovation landscape is rapidly expanding, supported by world-class research institutions and collaborative incubators. Organizations such as the Manitoba Technology Accelerator (MTA) and regional innovation hubs across British Columbia and Ontario offer ideal environments for early-stage medtech development.
2. Strong Clinical and Ethical Standards
Canada’s medical research framework emphasizes patient safety, ethical testing, and clinical transparency. These align perfectly with our values at PainSense, developing technology that not only innovates but also earns the trust of clinicians and patients alike.
3. Pathways to Certification and Market Readiness
To scale responsibly, a health-tech company needs clear regulatory and quality standards. Canada’s structured path toward Health Canada certification and international ISO compliance provides the roadmap we need for global credibility. We see Canada not just as our operational base, but as a gateway to future international expansion.
Looking Ahead: Our Next Steps
The coming months will be crucial for PainSense. Here’s what’s next on our roadmap:
Patent and Intellectual Property Protection
We are preparing to file for patent protection on our device’s core methodology and design. This will safeguard our intellectual property and solidify our position as pioneers in objective pain measurement.
Achieving ISO and Canadian Market Standards
PainSense is pursuing ISO certification and other required standards to ensure our device meets international safety and performance benchmarks. These certifications will also enable partnerships with hospitals, clinics, and research centers across Canada.
Beta Launch and Real-World Testing
Once the MVP is finalized, we will initiate a beta launch with selected hospitals and clinical partners. This phase will allow us to gather valuable data, refine user experience, and validate performance in diverse care environments. Feedback from clinicians and patients will directly influence our next design iterations.
Collaboration and Knowledge Exchange
As our network grows, we aim to foster open collaboration with physicians, anesthesiologists, dentists, and pain researchers. Pain assessment is a universal challenge, and progress comes fastest when we share insights across disciplines.

Join PainSense on This Journey
We believe innovation in healthcare thrives on collaboration and conversation. Every clinician’s experience, every patient’s story, and every piece of feedback brings us closer to creating a future where pain is truly understood and managed.
👉 Share your thoughts in the comments :
What challenges have you faced in pain assessment? What would make your clinical workflow easier? Your perspective helps us shape a tool designed for real-world needs.