The Newest Technologies You Should Know
In recent years, we have witnessed remarkable innovations in pain assessment technology. Traditional pain scales that rely on patient self-report are giving way to high-tech solutions that promise more objective and precise measurements. In this post, we explore the state of pain assessment tech in general, and share how PainSense – our own solution – is transforming pain measurement, from its early MVP prototype to the latest improvements in our device.

The Latest Advances in Assessment Technology
For decades, measuring a patient’s pain largely meant asking “How bad is your pain on a scale of 1 to 10?” or interpreting facial grimaces. Such subjective methods are notoriously unreliable – they depend on individual pain tolerance and communication ability, often leading to misjudgments in treatment. In fact, standard pain-rating techniques can be imprecise and heavily reliant on a patient’s ability to communicate . This has driven a surge of interest in technologies that bring objectivity to pain assessment. Key advancements include:

Sensor-Based Devices for Objective Pain Measurement
Innovative medical devices are being developed to quantify pain through physiological responses. For example, AlgometRx’s Nociometer® uses applied stimuli to objectively measure pain levels, allowing physicians to choose appropriate medications and dosages based on data rather than guesswork . Such tools convert a patient’s response (e.g. to pressure or other stimuli) into a numeric pain score, addressing the communication gaps of traditional scales.

The Role of Computer Vision in Smart Diagnostics
Artificial intelligence is enabling pain assessment in populations who struggle to self-report, like young children or cognitively impaired patients. A prime example is the PainChek® system, the first regulatory-cleared pain assessment app, which uses AI-driven facial recognition to analyze micro-expressions and quantify pain in real time . By detecting subtle facial muscle movements associated with pain, these tools provide an objective pain score that caregivers can trust, even if the patient cannot describe their pain verbally.

Neuroimaging and Biomarkers to Objectively Measure Pain
Researchers are also exploring high-tech clinical tools to measure pain more directly. Techniques like fMRI and EEG can visualize or detect the brain’s response to painful stimuli, offering real-time insights into the subjective experience of pain . Meanwhile, biological markers (hormone levels, inflammatory markers, etc.) are being studied for correlations with pain intensity. Combined with machine learning algorithms to interpret complex data, these approaches are paving the way for pain assessments that are data-driven and personalized . In short, emerging science is turning pain into something that can be seen or measured objectively, rather than just asked about.
The Future of Pain
These advancements all strive for one goal: a future where pain can be quantified and managed with far greater precision than ever before. We are moving from an era of “pain is what the patient says it is” to one where pain has measurable signatures – whether through a device reading, an algorithm’s analysis, or a brain scan. This evolution not only improves accuracy in diagnosis and treatment, but also holds promise for more equitable pain management (e.g. reducing biases and disbelief in patients’ reported pain) through objective data.
PainSense: Bringing Objectivity to Pain Measurement
PainSense was born out of this need for a more reliable way to measure pain. We developed PainSense to quantify pain levels in a simple yet effective manner – our technology brings objectivity to pain assessment by turning applied pressure from a patient into a precise numerical data point . In practice, the patient uses our device (for example, by squeezing a handheld sensor), and the device converts that pressure into a pain score. This is a leap forward from the traditional self-reported scales: instead of guessing a number on a pain scale, patients physically communicate their pain tolerance, and PainSense captures it as data. By removing much of the guesswork, we empower healthcare providers to tailor treatments with unprecedented accuracy based on real measurements rather than subjective impressions.
PainSense is designed to be compact and user-friendly, making it viable across hospitals, clinics, and even home care settings . We often say PainSense is not just a device, but a movement – it represents a new approach to pain management that prioritizes objective, data-driven care. Our goal is to set new standards in pain assessment and ultimately improve patient outcomes . When caregivers have reliable pain metrics, they can make more informed decisions: for instance, adjusting medication dosages more precisely or identifying when an intervention is truly helping. In the long run, we believe this will lead to better pain relief with fewer side effects and a reduction in issues like pain being dismissed or under-treated.

From Prototype to MVP: How PainSense Turned an Idea into a Working Solution
Building the first PainSense prototype and MVP was an exciting challenge. We started with a simple concept: a device that a patient could squeeze or press to indicate pain intensity, which would then output a number. Turning that idea into a working minimum viable product (MVP), however, was no small feat. We faced significant hurdles in developing a tool that was both practical (usable in real healthcare environments) and accurate enough to trust. Translating a physical force (the pressure of a hand squeeze) into reliable, consistent data required extensive research and development work . Early on, we had to answer questions like: What kind of sensor should we use to capture the pressure? How do we calibrate the device for different patients? How do we account for the fact that everyone’s hands and strength are different? Solving these issues meant many long hours of engineering and iteration.
IDEA
MVP
PRODUCT
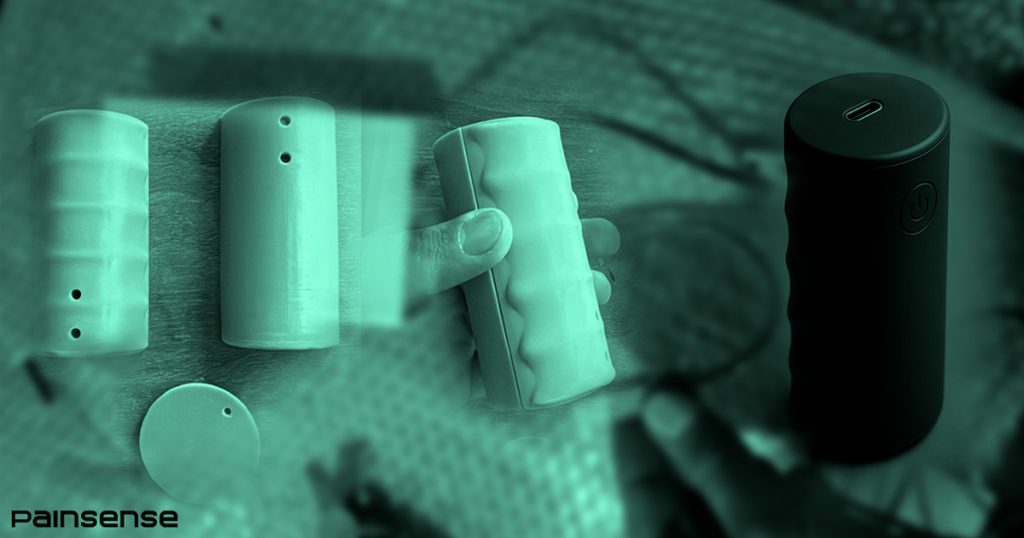
Our initial MVP prototype was quite basic – essentially a proof-of-concept device. We built it to demonstrate that the core idea works: that when a patient squeezes the device, we can generate a numeric pain score that correlates with their perceived pain. This rudimentary prototype allowed us to start testing and gather feedback. We learned a lot from these early trials. In fact, each prototype iteration provided valuable insights, which we fed back into the design. The early prototypes underwent rigorous testing to ensure they could deliver consistent results in a clinical setting . For example, we would apply known forces and compare the device’s readings, or have volunteers use it and report their pain to see if the numbers made sense. With each round of testing, we discovered ways to improve both the hardware and the software algorithms inside the device .
Some of the key improvements in those early stages included reinforcing the device’s build (so it wouldn’t break under a strong grip), fine-tuning the pressure sensor’s sensitivity, and smoothing out the software that translates pressure into a pain score. We also paid attention to user comfort and ease of use. Initially, our prototype was a bit clunky – think of something like a modified blood pressure squeeze ball with wires attached. Over time, we refined the shape and materials to make it more ergonomic for patients of all ages. By the end of this early development journey, our MVP had evolved from a crude gadget into a more polished device that could consistently perform its job. This was a critical milestone: it proved that objective pain measurement is not only theoretically possible, but also practically achievable in real-world scenarios.
Improving the MVP
Fast forward to today – our MVP has come a long way from that first prototype. In the latest iteration of PainSense, we’ve implemented major improvements that bring us closer to a production-ready product. It’s fair to say the device has gone “from prototype to purpose-built,” meaning it’s no longer just a concept demo; it’s been engineered with real-world use in mind. One of the most visible advancements is in the design and ergonomics of the device. The latest PainSense model has a sleek, compact form factor shaped by feedback from earlier versions. Patients can comfortably hold and use it, and clinicians find it intuitive to operate. The device is wireless and portable, which is important for use at the bedside or in a busy clinic environment. We’ve also chosen durable, medical-grade materials for the casing so that it withstands repeated use and disinfection – critical for hospital settings.

Capturing Pain More Precisely
Under the hood, we’ve upgraded the sensor and algorithm that power PainSense. The pressure sensor now offers higher precision and stability, improving the accuracy of each pain measurement. We recalibrated our system based on extensive testing data, so the numeric scores it produces align even more closely with patient pain reports and known pain stimuli thresholds. Our engineering team also refined the firmware (the on-device software) which processes the input. The result is faster response times and a smooth, real-time readout of pain levels as the patient uses the device. These changes mean PainSense can capture subtle differences in pain intensity that earlier versions might have missed, giving healthcare providers a more nuanced understanding of a patient’s pain profile.
Another important set of enhancements in the MVP is related to data handling and integration. In the initial prototype phase, data might have been collected manually or on a rudimentary interface. Now, our MVP can synchronize with a companion software application. We have developed an app interface that pairs with the PainSense device to log pain scores over time, visualize trends, and integrate those readings into a patient’s digital health record. This is a stepping stone to the fully connected vision we outlined earlier. It means that when a patient uses PainSense, their pain data can be securely saved and later reviewed by their doctor, or even analyzed to spot patterns (for example, to see if a new medication is reducing their daily pain levels). Real-time monitoring is also improved – a clinician can watch the pain level readings live on the app as the patient uses the device, which is very useful in procedures or therapy sessions.

We shared a glimpse of these MVP advancements on our social media recently, and the response has been energizing. Our community has seen the side-by-side comparison of the early prototype and the current device, and the difference is striking. The latest PainSense device truly embodies our dedication to iterative improvement. Every tweak and upgrade was driven by what we learned in testing and by listening to feedback from healthcare professionals. We’re proud that our MVP is no longer just an experimental gadget, but a reliable tool that demonstrates how objective pain assessment can work in practice. Of course, the journey isn’t over – we will continue to iterate and refine. But with these latest changes, we’re closer than ever to bringing a finalized PainSense device to the market, one that could make a real difference in how pain is measured and managed for patients everywhere.